Planning for an infertility treatment like in vitro fertilization (IVF) is a significant step toward realizing your dream of becoming a parent—and it takes time, energy, and considerate planning. An IVF cycle calendar is one tool that can help.
Whether you’re considering IVF as an option, have just started your IVF journey, or are well into the process, creating an IVF calendar can help you know what to expect of your treatment so that you can better plan for and manage your treatment—and ultimately achieve a successful pregnancy.
How do you determine an IVF calendar?
Like many infertility treatments, IVF often involves a complex of hormone therapies, medications, and coordinating fertility treatments. With so many moving parts and diverging timelines, creating an IVF timeline calendar isn’t quite as simple as mapping out the IVF cycle itself.
The IVF process from start to finish depends on your specific goals and infertility diagnoses. Some intended parents, for example, might be using an egg donor, sperm donor, or gestational carrier to build their family with IVF. This involves coordinating with a surrogacy agency, egg donor program, or sperm bank; choosing your donor or surrogate, and legally securing the third party.
The timeline for this process varies widely, ranging anywhere from two weeks to secure a sperm donor to several months to secure a gestational carrier—depending on factors like your family’s personal third-party requirements, the availability of donors or gestational carriers, and whether you’re working with an external or in-house donor program.
Another preliminary process is pre-genetic carrier screening. Some parents choose to test their carrier status for genetic health conditions, either informing their donor selection or their selection of a healthy embryo later in the process. Depending on your IVF centre, it typically takes 1–2 weeks to receive these test results.
When it comes to the IVF cycle itself, there is still plenty of timeline variability from one family to the next—depending on personal health factors, third-party factors, and whether your treatment involves a fresh or frozen embryo transfer.
Your fertility specialist will help you create a more precise timeline, but to begin creating an IVF calendar or to get a general sense, you can work from the time ranges involved in a typical IVF cycle, which begins in coordination with your menstrual cycle.
What does a realistic IVF calendar look like?
A full round of IVF spans one menstrual cycle (1 month) for a fresh embryo transfer and at least two menstrual cycles (2 months) for a fresh cycle followed by a frozen embryo transfer cycle.
Frozen embryo transfer (FET) is the more common option for several reasons, including lower cost, reduced strain on the parent’s body, the option for preimplantation testing of embryos (PGT), and the potential for multiple embryos which can be cryopreserved.
After retrieving and freezing embryos, intended parents can choose to wait any amount of time before beginning the FET cycle, but for the sake of presenting one continuous IVF calendar and timeline range, we’ll walk through the stages of the IVF cycle assuming no additional waiting times.
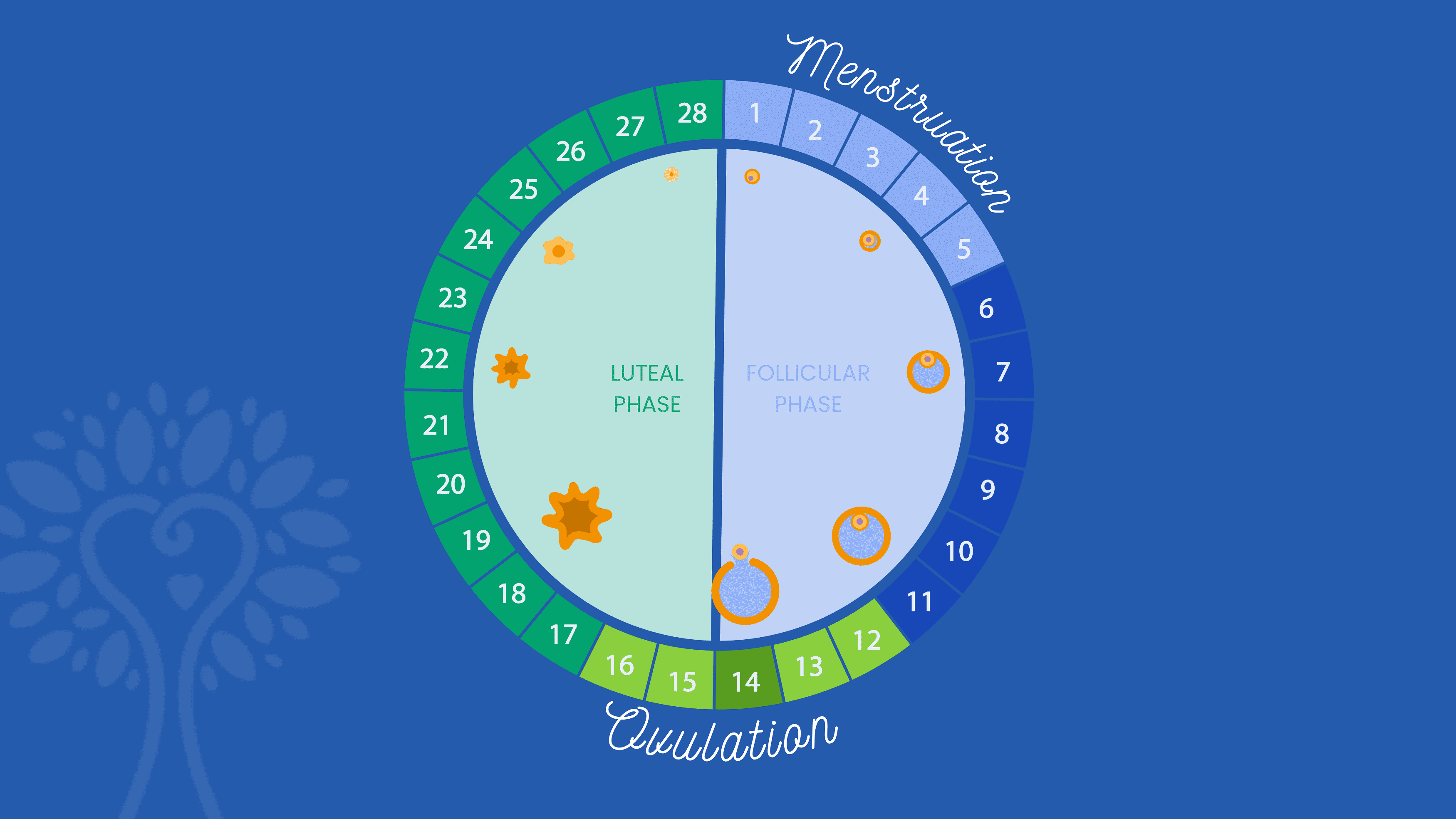
Assuming Day 1 is the first day of your menstrual cycle, here’s what a typical IVF calendar will include:
Day 2–3
Ovarian Stimulation: The IVF cycle starts with a 9–15 day period of ovarian stimulation, using hormone injections called gonadotropins or follicle stimulating hormones, to produce multiple follicles and allow as many eggs as possible to mature for retrieval from the ovaries. Sometimes birth control pills or estrace are prescribed for you to take prior to starting the follicle stimulating hormones.
Monitoring: Throughout the ovarian stimulation phase, regular monitoring through ultrasounds and blood tests is conducted to track follicle growth and hormone levels and to inform any adjustments to medication dosages or changes in your IVF calendar.
Day 9–15
Trigger Injection: Once a sufficient number of follicles have reached maturity, a different gonadotropin injection is administered to induce final egg maturation.
Day 11–17
Egg Retrieval: The egg retrieval procedure is performed as an outpatient procedure under sedation or anesthesia. A needle is used to extract the mature eggs from the ovaries.
Sperm Collection and Fertilization: Sperm is either collected on the same day as the egg retrieval or cryopreserved earlier for later use. Once the eggs are retrieved and the sperm collected, both are transferred to an embryology lab where they are fertilized and closely monitored by embryologists.
Beginning of Embryo Culturing: Once fertilized, the embryos are cultured in the lab for 5–7 days, until they reach the blastocyst stage, at which point embryologists evaluate the embryos’ quality to determine which can be used. At this point, viable embryos can either be transferred back into the uterus directly or frozen for FET and/or PGT.
Day 20–27 (Optional – FET only)
Preimplantation Genetic Testing (PGT): Often informed by a genetic risk found during the earlier carrier screening, PGT allows parents to test the carrier status and chromosomal health of each embryo. The embryos are biopsied and sent into a lab for testing, which typically takes 1–2 weeks.
Day 16–21
Beginning of Uterine Preparation: In the case of an FET, the parent or gestational carrier undergoes 3–4 weeks of hormone treatments to enhance the uterine receptivity and support the early stages of pregnancy. This involves 2–3 weeks of estrogen treatments, followed by progesterone.
The embryo transfer is commonly done on the 6th day of progesterone. For a fresh embryo transfer, progesterone treatment is typically started within 24 hours of the egg retrieval and continues throughout the first trimester.
Day 21–49
Embryo Transfer: On the 6th day of progesterone treatment, the fresh or thawed embryo is transferred to the uterus.
Day 31–63
Pregnancy Test: Approximately 10–14 days after the embryo transfer, a blood test is performed to determine if pregnancy has been achieved.
How long do you have to wait after a failed round of IVF?
Experiencing a failed round of IVF—whether at the egg retrieval or embryo transfer stage—can be very discouraging and emotionally painful. Fortunately, there are often several treatment adjustments and therapeutic additions that can be made to increase odds of success in the next round. Before beginning the next IVF cycle attempt, it’s important to wait at least one menstrual cycle.
This waiting period, which typically amounts to about 4 weeks, allows the body to recover from the hormonal stimulation and any procedures associated with the previous cycle, ensuring a more stable and receptive uterine environment for the next attempt.
Like most aspects of your IVF calendar, it’s important to note that the specific waiting time may be different for each person, and your fertility specialist may recommend more based on your medical history and the reasons for the previous IVF failure.
Creating an IVF Calendar with ICRM
No matter where you find yourself on your fertility journey, the Idaho Center for Reproductive Medicine is here to provide support, guidance, and tailored treatment for your unique family.
During an IVF treatment with ICRM, our dedicated coordinators work closely with you to create and maintain an IVF calendar, schedule appointments, and navigate the intricacies of your treatment to help you achieve a successful pregnancy.






